Multi-infarct dementia
| Multi-infarct dementia | |
|---|---|
| Classification and external resources | |
| ICD-10 | F01.1 |
| ICD-9 | 290.4 |
| DiseasesDB | 8393 |
| eMedicine | med/3150 neuro/227 |
| MeSH | D015161 |
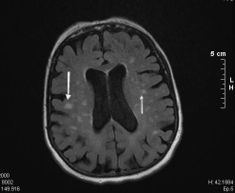
Multi-infarct dementia, also known as vascular dementia, is the second most common form of dementia after Alzheimer's disease (AD) in older adults.[1] The term refers to a group of syndromes caused by different mechanisms all resulting in vascular lesions in the brain. Early detection and accurate diagnosis are important, as vascular dementia is at least partially preventable.
The main subtypes of this disease are: mild cognitive impairment, multi-infarct dementia, vascular dementia due to a strategic single infarct (affecting the thalamus, the anterior cerebral artery, the parietal lobes or the cingulate gyrus), vascular dementia due to hemorrhagic lesions, small vessel disease (which includes vascular dementia due to lacunar lesions and Binswanger's disease), and mixed Alzheimer's and vascular dementia.
Vascular lesions can be the result of diffuse cerebrovascular disease or focal lesions (or a combination of both, which is what is observed in the majority of cases). Mixed dementia is diagnosed when patients have evidence of AD and cerebrovascular disease, either clinically or based on neuroimaging evidence of ischemic lesions. In fact vascular dementia and Alzheimer's disease often coexist, especially in older patients with dementia.
Contents |
Epidemiology
Vascular dementia is the second most common cause of dementia in the United States and Europe in the elderly, but it is the most common form in some parts of Asia. The prevalence of the illness is 1.5% in Western countries and approximately 2.2% in Japan. It accounts for 50% of all dementias in Japan, 20% to 40% in Europe and 15% in Latin America. The incidence of dementia is 9 times higher in patients who have had a stroke than in controls. 25% of stroke patients develop new-onset dementia within 1 year of their stroke. The relative risk of incident dementia is 5.5% within 4 years of suffering a stroke.
The prevalence of vascular dementia is higher in men than in women and it increases with age.
Mortality/morbidity
The 5-year survival rate is 39% for patients with vascular dementia compared with 75% for age-matched controls. Vascular dementia is associated with a higher mortality than "Alzheimer's", presumably because of the excess in cardiovascular risk factors.
Clinical presentation
Patients suffering from vascular dementia present with cognitive impairment, acutely or subacutely, after an acute cerebrovascular event. After the onset a stepwise progression is typical. However stepwise progression may not be observed in small vessel disease, Binswanger's disease or vascular dementia due to small lacunar infarcts.
In small vessel disease the incidence peaks between the 4th and the 7th decades of life and 80% will have a history of hypertension. Patients develop progressive cognitive, motor and behavioral signs and symptoms. A significant proportion of them also develop affective symptoms. These changes occur over a period of 5–10 years. If the frontal lobes are affected, which is often the case, patients may present as apathetic or abulic. This is often accompanied by problems with attention, orientation and urinary incontinence.
As already stated, small vessel disease and focal lesions often overlap, so these two patterns may be evident in the same individual concurrently.
Rare genetic disorders which result in vascular lesions in the brain have other patterns of presentation. As a rule of thumb they tend to present earlier in life and have a more aggressive course.
Diagnosis
Several specific diagnostic criteria can be used to diagnose vascular dementia,[2] including the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria, the International Classification of Diseases, Tenth Edition (ICD-10) criteria, the National Institute of Neurological Disorders and Stroke- Association Internationale pour la Recherche et l'Enseignement en Neurosciences (NINDS-AIREN) criteria,[3] the Alzheimer's Disease Diagnostic and Treatment Center criteria, and the Hachinski ischemic score.[4]
Lateralizing signs such as hemiparesis, bradykinesia, hyperreflexia, extensor plantar reflexes, ataxia, pseudobulbar palsy, and gait and swallowing difficulties may be observed.
In terms of cognitive testing patients have patchy deficits. They tend to have better free recall and fewer recall intrusions compared with patients with Alzheimer's disease. As small vessel disease often affects the frontal lobes, apathy early in the disease is more suggestive of vascular dementia because it usually occurs in the later stages of Alzheimer's. Consequently patients with vascular dementia perform worse than their Alzheimer's disease counterparts in frontal lobe tasks such as verbal fluency. They also tend to exhibit more perseverative behavior. They may also present with general slowing of processing ability, difficulty shifting sets and impairment in abstract thinking. In the more severe patients, or those patients affected by strategic infarcts in the Wernicke or Broca areas, dysarthrias, dysphasias and aphasias may be present.
Etiology
Risk factors for vascular dementia include hypertension, smoking, hypercholesterolemia, diabetes mellitus, and cardiovascular and cerebrovascular disease.
Investigations
The recommended investigations for cognitive impairment should be carried out, including a dementia screening blood test, chest X-Ray, CAT scan and EKG. The screening blood test should typically include full blood count, liver function tests, thyroid function tests, lipid profile, erythrocyte sedimentation rate, C reactive protein, syphilis serology, calcium serum level, fasting glucose, urea and electrolytes, vitamin B-12, folate. In selected patients HIV serology and autoantibody testing may be done.
Treatment
The aim of the management is the prevention of further cerebrovascular lesions. This includes administering antiplatelet drugs and controlling major vascular risk factors (hypertension, hypercholesterolemia, smoking and diabetes mellitus to mention a few).
The general management of dementia includes referral to community services, judgment and decision-making regarding legal and ethical issues (e.g., driving, capacity, advance directives), and consideration of caregiver stress.
Cholinesterase inhibitors such as galantamine have shown to be helpful in various randomized controlled trials. However their use is not licensed yet for this indication.
Behavioral and affective symptoms are particularly important in this patient group and deserve special consideration. These problems, if they develop, tend to be resistant to conventional psychopharmacological treatment and in many cases lead to hospital admission and placement in permanent care. Agents that may be useful include antidepressants, neuroleptics and mood-stabilizers. Electroconvulsive therapy may be indicated in extreme cases provided a medical contraindication does not exist.
See also
- Cerebrovascular accident
- Binswanger's disease
References
- ↑ "Vascular Dementia: A Resource List". http://www.nia.nih.gov/Alzheimers/Publications/vascular.htm.
- ↑ Wetterling T, Kanitz RD, Borgis KJ (January 1996). "Comparison of different diagnostic criteria for vascular dementia (ADDTC, DSM-IV, ICD-10, NINDS-AIREN)". Stroke 27 (1): 30–6. PMID 8553399. http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=8553399.
- ↑ Tang W, Chan S, Chiu H, Ungvari G, Wong K, Kwok T, Mok V, Wong K, Richards P, Ahuja A (2004). "Impact of applying NINDS-AIREN criteria of probable vascular dementia to clinical and radiological characteristics of a stroke cohort with dementia". Cerebrovasc. Dis. 18 (2): 98–103. doi:10.1159/000079256. PMID 15218273.
- ↑ Pantoni L, Inzitari D (1993). "Hachinski's ischemic score and the diagnosis of vascular dementia: a review". Italian journal of neurological sciences 14 (7): 539–46. doi:10.1007/BF02339212. PMID 8282525.
External links
- Helpguide article on vascular dementia
- J Bowler & V Hachinsky, Vascular Cognitive Impairment: Preventable Dementia, Oxford University Press 2003, ISBN 0-19-263267-1.
- Multi-Infarct Dementia Fact Sheet at ninds.nih.gov
- Multi-Infarct Dementia at nmha.org
- Vascular Dementia: Symptoms, Prognosis, and Support at helpguide.org
- American Academy of Neurology (2007, December 21). Walking And Moderate Exercise Help Prevent Dementia. ScienceDaily. Retrieved December 21, 2007, from http://www.sciencedaily.com/releases/2007/12/071219202948.htm
- What is vascular dementia? Alzheimer's Society fact sheet
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||